Behavior Change Rewards Platform for Healthcare Insurance Company
Led design of a rewards platform that increased preventative care engagement by 2.67x (from ~3% to 8%), delivering an estimated $10M+ in healthcare cost savings. The year-long initiative transformed member perception from viewing the app as a transactional tool to a trusted health partner.
Role: Lead UX Designer | Timeline: ~1 year | Year: 2019-2020
Situation: A major healthcare insurer faced ~3% engagement with behavior change campaigns designed to encourage preventative care. Members viewed their apps as purely transactional (claims, provider search) and questioned why the company recommended specific health actions. Low engagement resulted in higher healthcare costs as preventative care was missed and members used expensive care sites.
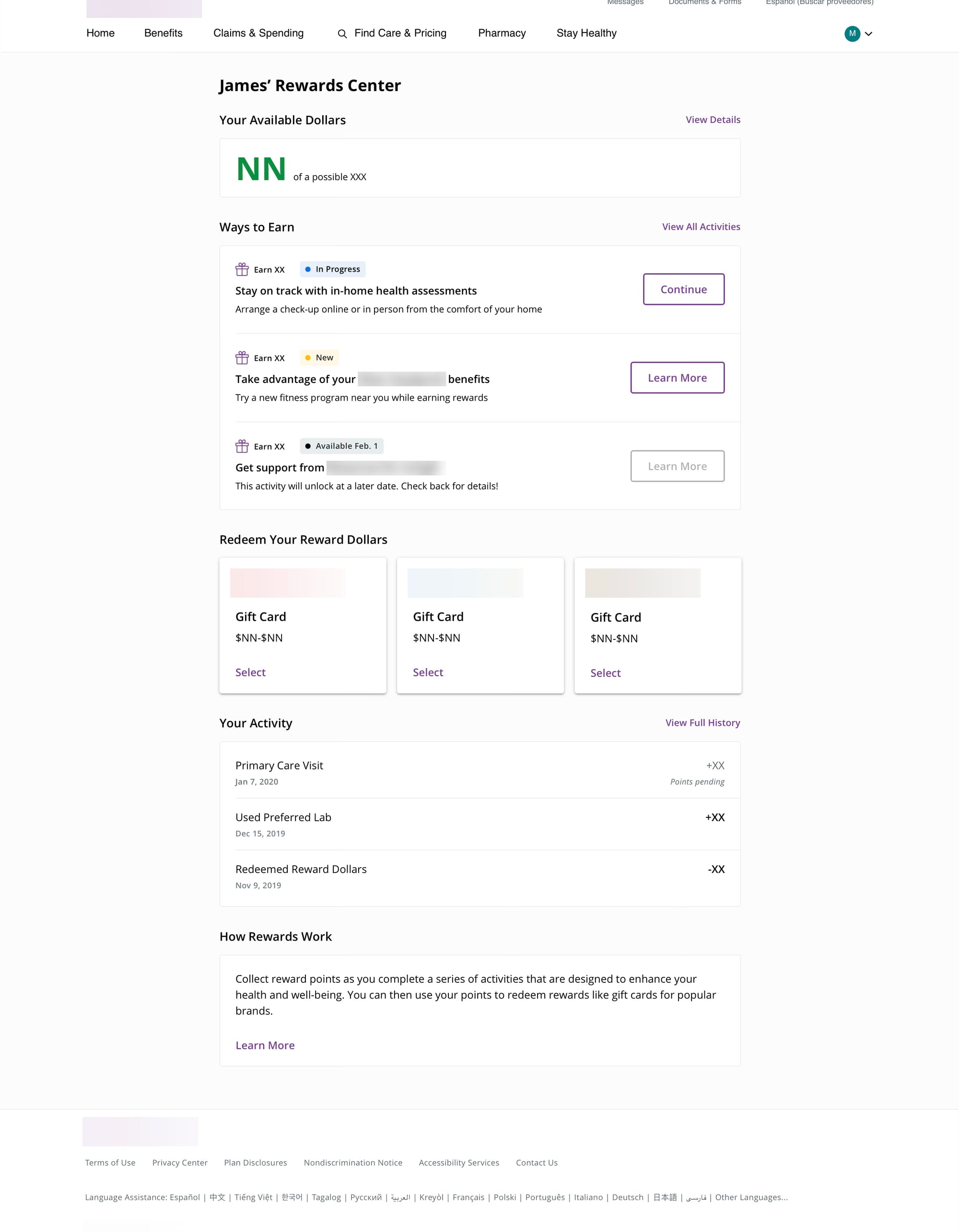
Task: Lead UX design for a rewards platform that would increase campaign engagement while giving members autonomy and transparency, ultimately reducing healthcare costs for both the business and members.
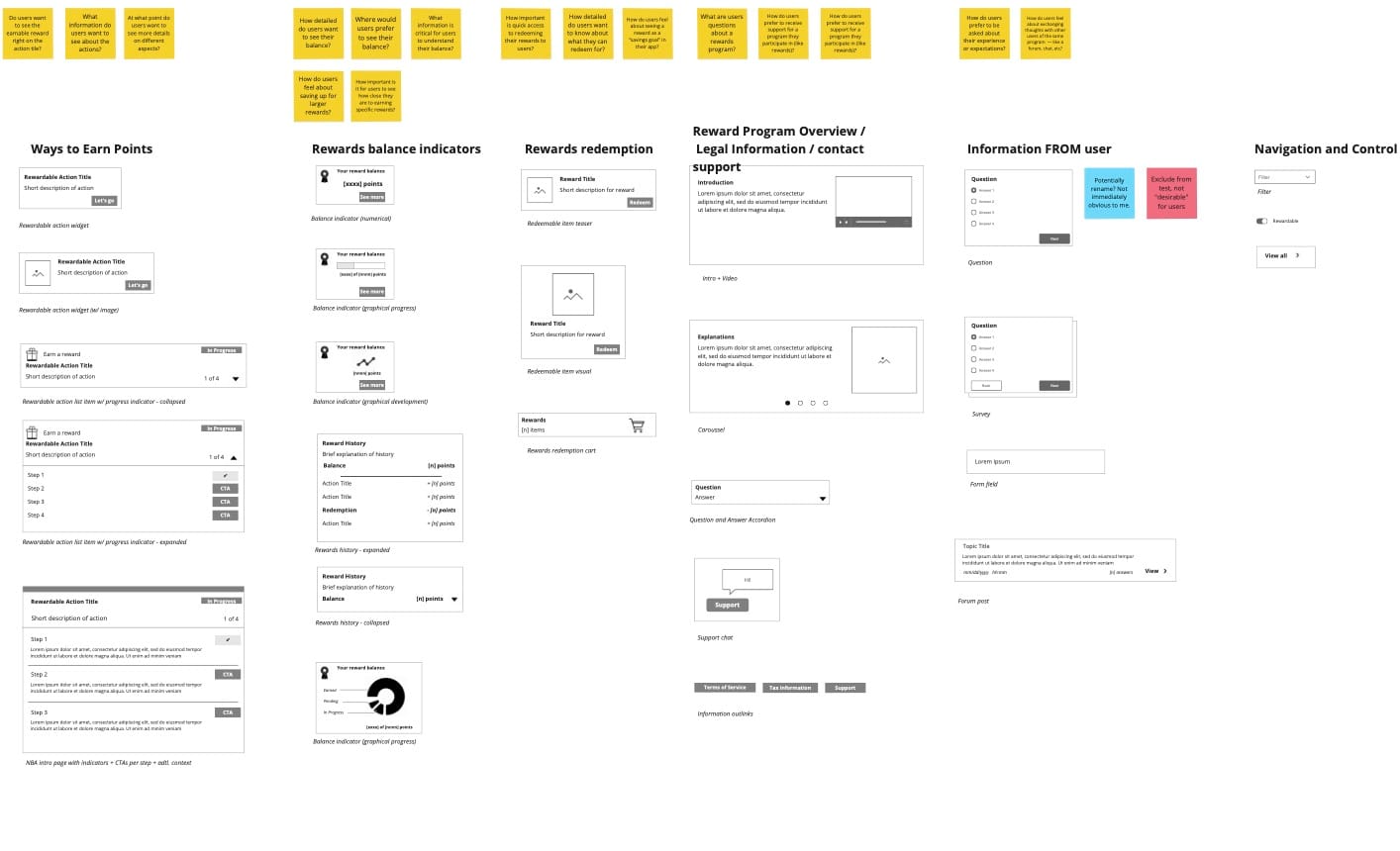
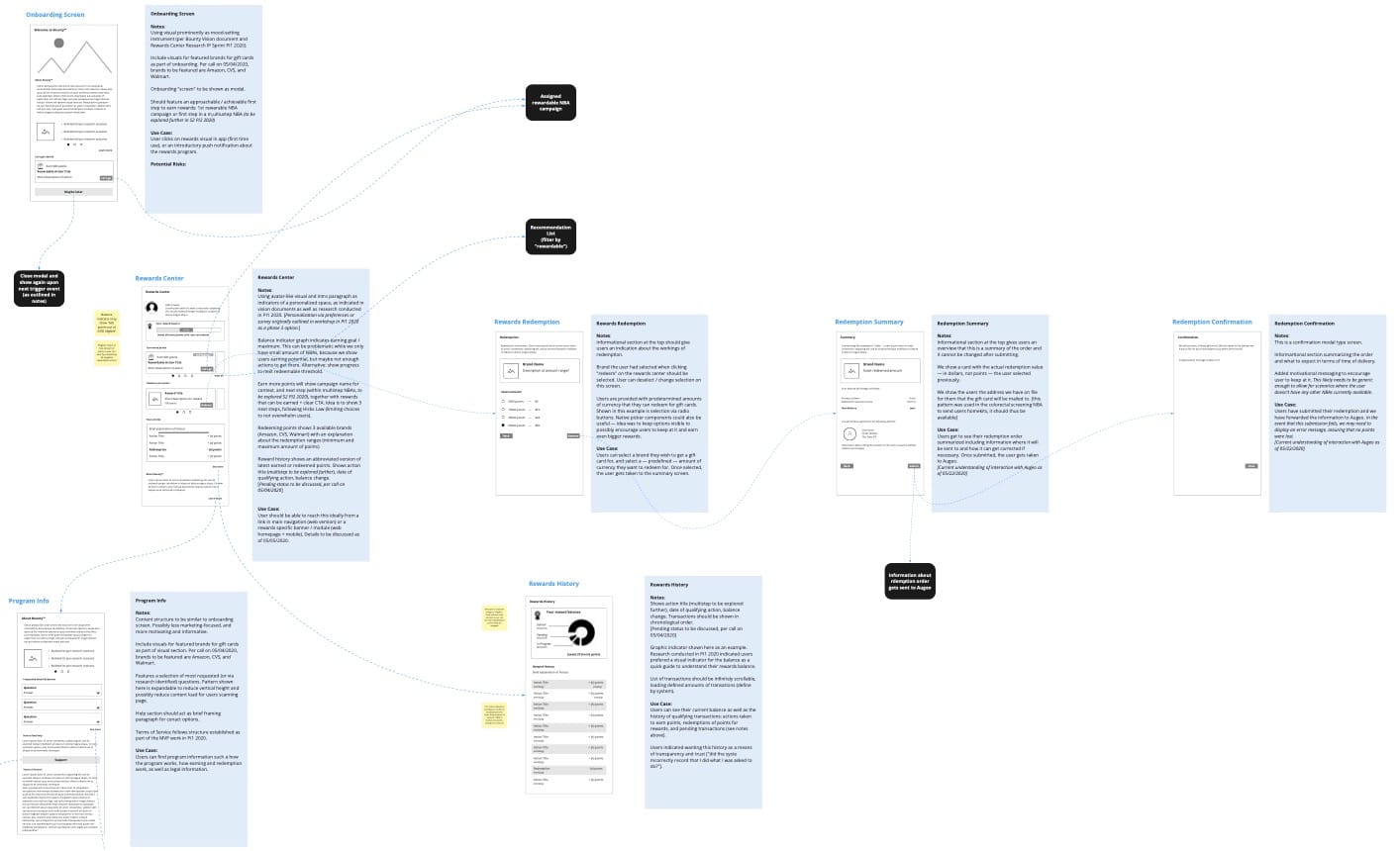
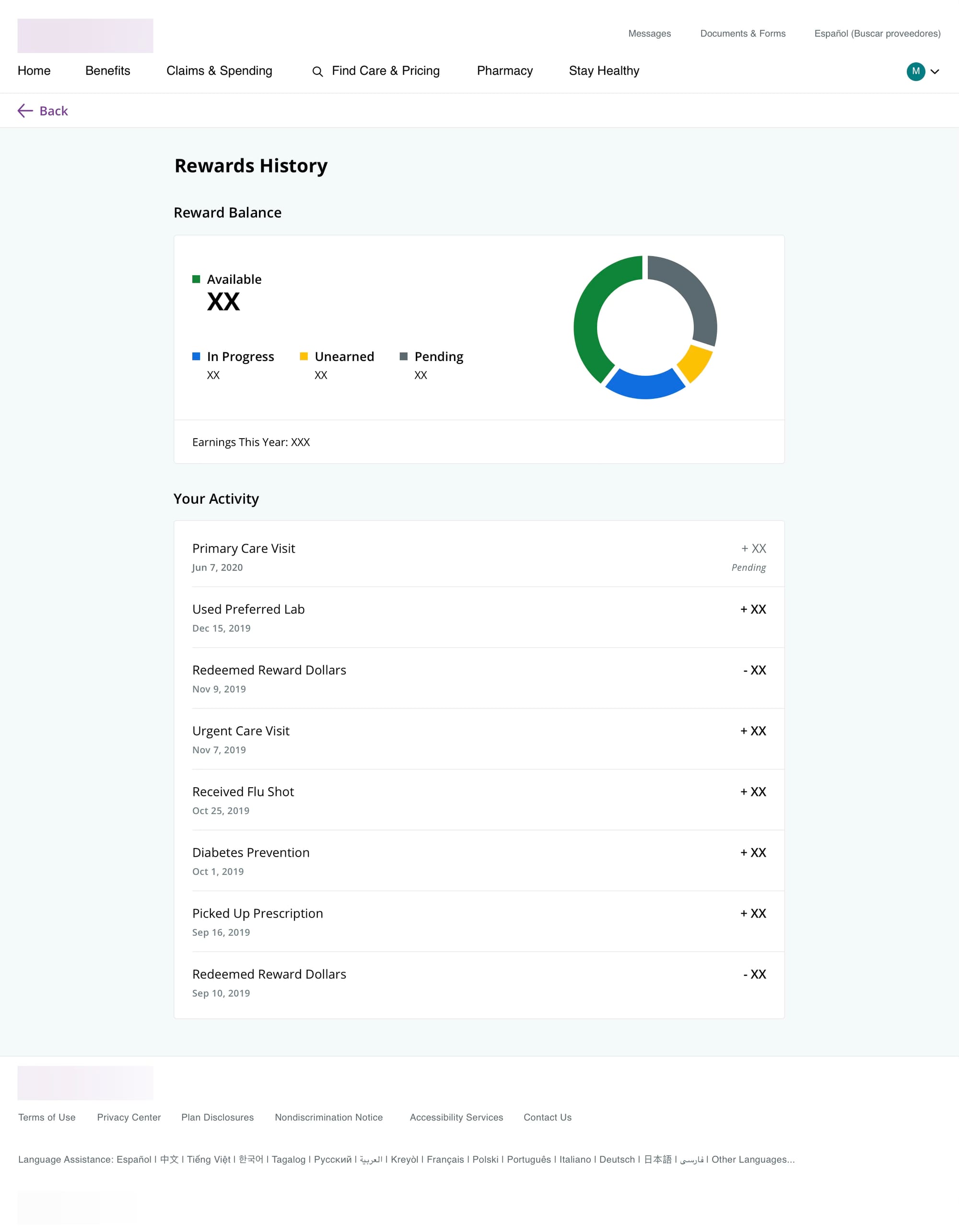
Action: I led a cross-functional team including UI designer, content strategist, and UX researcher. Leveraging longitudinal studies and competitive analysis, I discovered transparency and autonomy were critical for member trust. I designed a centralized Rewards Center as the dedicated hub for behavior change campaigns, created campaign microsites offering alternative entry points, and built member autonomy controls allowing users to pause or archive actions. I calibrated reward values to action effort (vaccine shot vs. multi-week therapy program) and focused all campaign messaging on health benefits rather than rewards. I collaborated with accessibility teams to ensure compliance across visual, interaction, and plain language standards throughout the year-long development.
Result: The platform achieved a projected 2.67x engagement improvement (from ~3% to minimum 8%) with behavior change campaigns, directly impacting healthcare cost reduction for both the business and members. By transforming the app from a "transactional billing tool" to a "health partner," the design enabled members to take preventative actions that avoided more expensive critical care later. The estimated impact included $10M+ in savings by preventing costly downstream procedures through increased screening participation, medication adherence, and lifestyle changes. The success demonstrated that user autonomy and transparent communication were more powerful engagement drivers than rewards alone.
Always looking to help create innovative solutions. If you have a project you'd like help with or if you want to learn more about this project or others, don't hesitate.
